AVer Connected Health Solutions: Tele-ICU
AVer Auto Tracking Camera and PTZ Management utilities, deployed in the nurse station of ICU, alleviate the strain on medical professionals.
AVer Auto Tracking Camera and PTZ Management utilities, deployed in the nurse station of ICU, alleviate the strain on medical professionals.
AVer MD330U Series Cameras are specially designed and medically certified for Telemedicine with the IEC 60601-1-2 Medical Certification.
Medical diagnostic displays are equipped with advanced features to enhance precision and accuracy in medical imaging. These features include the 16bit LUT, DICOM Calibration, Full Screen Uniformity, Lightbox Mode, Ambient Light Adaptive, SmarTouch, Integrated Front Sensor, JUSHA QA Compatibility, Human Detection, Jusha Shark Gill Design, Energy Efficiency, Multi-stance Stand, CGA Technology, and Spotlight Mode. Each of these technologies plays a crucial role in ensuring high-quality imaging, which is essential for accurate diagnosis and effective treatment planning.
The JUSHA-C820G monitor is designed to meet the highest standards in medical imaging. With features like DICOM calibration, integrated front sensors, and ambient light adaptation, it ensures accurate and reliable diagnostics. In this blog post, we’ll explore these features in detail and how they contribute to superior medical imaging.
!DICOM Calibration
The JUSHA-C820G monitor complies with the DICOM 3.14 standard and includes a dynamic LUT. This ensures accurate and stable lesion diagnosis at any brightness, contrast, and color temperature. For more details on DICOM standards, you can visit DICOM Standards.
!Integrated Front Sensor
Users can customize the black point, white point, and environmental brightness of the DICOM curve. Additionally, built-in sensors measure display brightness in real-time, automatically adjusting to the best settings and complying with DICOM standards. Learn more about our sensor technology.
!JUSHA Qualitas QA
Users can check and calibrate the monitor themselves, which reduces the effects of panel aging. Consequently, this prolongs the monitor’s lifespan and ensures more accurate images. Discover more about JUSHA Qualitas QA.
!Independent Dual Input Setup
You can independently change the image settings for different video sources, such as calibration mode, resolution, and color depth. Thus, different image modes meet various requirements. Check out our video input options.
!Ambient Light Adaptive
The monitor measures ambient light in real-time and adjusts the display accordingly to ensure accurate diagnosis. For further reading on ambient light sensors, visit Ambient Light Sensors.
!SmarTouch
Medical image diagnosis often requires high brightness, which can damage eyesight with long-term use. To solve this, we offer a one-key brightening function. You can switch the display brightness between normal and maximum with a simple shortcut key, thereby providing great convenience. Learn more about SmarTouch technology.
!X-ray Film View
The XFV can increase the monitor’s brightness to its peak value, replacing the traditional Lightbox for film reading and, as a result, increasing work efficiency. Find out more about X-ray Film View.
The JUSHA-C820G monitor is a powerful tool for medical imaging, offering a range of features that ensure accuracy, reliability, and convenience. By integrating advanced technologies like DICOM calibration, integrated front sensors, and ambient light adaptation, it sets a new standard in medical diagnostics.
For more information, visit our product page. JUSHA-C820G
By Maggie Chu

The rapid pace of technology adoption is occurring in all industries, including in healthcare. In large part due to the COVID pandemic preventing people from having in-person access to medical resources, the aid of technology has helped broaden the reach of practitioners and increase options for patients. In the year 2023, we will look at some recent trends in healthcare technology, including telehealth, automation, and wearable technology.

Telehealth has risen in importance due to COVID, but it also shines by providing those with fewer medical resources with a fast, efficient way of receiving medical treatment.
For instance, diabetics often require routine eye examinations by an ophthalmologist specializing in diabetic retinopathy, making it particularly difficult for older diabetics living in rural areas. Many manufacturers developed telehealth suitcases and telehealth carts, both of which are suitable for different application environments. The telehealth suitcase is suitable for emergency situations or pop-up clinics with limited space. It can hold a tablet, keyboard, speaker, and smaller medical devices like stethoscopes, wireless ultrasounds, and funduscopes. On the other hand, the telehealth cart is a great option for institutions in rural areas or with scarce resources to connect with specialized practitioners remotely. Generally, the telehealth cart comes with a high-definition PTZ camera, computer, and speaker along with an adjustable medical cart. This configuration allows for high-quality two-way communication for medical professionals to provide care remotely, saving patients time from long travel and waits in healthcare facilities.

Hospital workers are often overwhelmed in their daily routines, making automation a great choice for hospitals, with applications ranging from medical notetaking to sterilization.
Documenting a patient’s condition is a time-consuming, repetitive, yet necessary task for medical practitioners. With the rise of voice assistants, the input of this data can be simplified and completed automatically. Though doctors have long utilized medical transcription services and voice recognition technology to complete transcription tasks, AI-powered speech-to-text systems can now recognize and make clinical documentation during the consultation itself, so doctors can spend less time on administration and more time on patients, reducing clinical burnout and increasing patient satisfaction.
For hospital room sterilization, automation can also be used to ensure a sanitary environment for both patients and staff. Automated room disinfection (ARD) systems can reduce human errors, reduce the possibility of cross-infection, and free up time for hospital staff so they can focus on more pressing issues.

Wearable devices are changing the way we interact with our health, giving us real-time data on our physiological well-being regarding sleep, heart, blood oxygen levels, and other metrics. They help us keep track of our overall health conditions, playing a helpful role in disease prevention or even disease management. Particularly outstanding in the prevention of cardiovascular conditions like arrhythmia, hypertension, and strokes, we see a study using Fitbit trackers to predict undiagnosed atrial fibrillation patients. Other wearable devices capable of tracking patient health include glasses, shoes, and even clothing that Incorporate smart textiles. These innovations will give people a better sense of their own health and help people make healthier choices in their daily lives.
Health technology can help improve the lives of patients all over the world by making checkups easier and tracking health metrics while simplifying the workflows of physicians and nurses. Especially for areas with a shortage of physicians and nurses, these technologies can help doctors reach a larger patient base and provide high-quality care to patients.
As we see healthcare systems adopting these new technologies and making their institutions smarter to cope with healthcare challenges, practitioners and authorities alike should be aware of how to responsibly and ethically use these systems while being compliant with regulations. When we have advanced technology and proper regulations in place, we are sure to see a great step forward in the healthcare industry.
Maggie Chu is a Brand Communication Strategist at AVer Information, working out of Taipei, Taiwan. She crafts press releases, blog posts, and other marketing materials to support AVer’s global branding efforts. She has a black dog named Niuniu, who is ironically a scaredy cat.

By Stephanie Pan
We have covered both Telemedicine and Telehealth in our previous AVer Experts, but we still haven’t introduced a term that has been increasingly used in recent years, and that is “Connected Health”. At the moment, there is no standard or universally accepted definition of what Connected Health is; however, a commonly referenced definition was given by researchers Caulfield and Donnelly, in which they stated that “Connected Health encompasses terms such as wireless, digital, electronic, mobile, and telehealth and refers to a conceptual model for health management where devices, services or interventions are designed around the patient’s needs, and health-related data is shared, in such a way that the patient can receive care in the most proactive and efficient manner possible.” In other words, it can be seen as an umbrella term for concepts such as telehealth, telemedicine, mobile health (mHealth), and more. It can also be defined as connecting every stakeholder, whether it be doctors, nurses, or patients, through various technologies and means of sharing information in regard to the patient’s status and well-being.
With how rapid information and communication technologies are advancing, there is a paradigm shift in the healthcare industry, suggesting that predictive and pre-emptive healthcare solutions should not only be personalized but also pervasive. While there are a lot of topics that we can tackle regarding Connected Health, we will start off with the basics for today as an introduction to this new model of healthcare delivery that is enabled by technology.

To understand what Connected Health is, it’d be better to start by knowing its essential concept first. Connected Health is thought to be a more proactive model of healthcare delivery compared to its more traditional counterparts in the sense that medical technologies and services are designed around the patient’s needs. What this means is that it puts the patient at the center of the entire process, regardless of their location or circumstances. In doing so, Connected Health, or more specifically the tools of Connected Health, has the potential to not only empower clinicians with more efficient and up-to-date data but also encourage patient engagement by providing them with key information at the tip of their fingertips. Connected Health is also especially relevant today because of the ongoing global pandemic. Due to Covid-19, many healthcare deliveries are affected, causing patient management to be difficult to maintain. As such, Connected Health is becoming an indispensable source of these issues, especially for patients with the coronavirus or chronic illness that require routine follow-ups and monitoring. What’s more, is that evidence from meta-analyses and systemic reviews have already been reported to support this claim.

Aside from its relevance, Connected Health is also helpful in improving patient care and overall patient experience. As you’d probably guess, this is mostly achieved via the tools of Connected Health. Currently, the most common tools include mobile healthcare apps, wearable devices, connected medical devices, interoperable medical ICT systems, and remote patient monitoring technologies. Through these tools, the patient’s needs, and health status can be constantly monitored across different clinical settings, leading to earlier interventions and fewer possibilities of adverse events. Additionally, wearable devices and mobile apps can also help identify individuals that are at risk by monitoring their vital signs and symptoms in real-time. This information can then be shared with the healthcare professionals, allowing them to deliver preventative care in a proactive and timely manner. To top it off, patients having access to their health status also allows them to feel more in control, which in turn increases their self-efficacy and satisfaction.
While there is definitely room for growth and improvement in the future, Connected Health is undoubtedly a dynamic and fast moving area of digital health that holds the potential to transform healthcare for the better.
Last Updated: June 21, 2024

Stephanie Pan is a Brand Communication Strategist at AVer Information, working out of Taipei, Taiwan. She crafts press releases, blog posts, and other marketing materials to support AVer’s global branding efforts.
By Maggie Chu
AI is undoubtedly the biggest buzzword these days, since the release of ChatGPT last year and then reaching an all-time high at Nvidia CEO Jensen Huang’s Computex keynote. Now, people are anticipating what comes next for AI and what it can do for humanity, signaling an imminent change in how we as humans conduct our day-to-day lives.
In the past few months, we’ve seen more AI applications in the tech world, showcased in major exhibitions and used in everyday consumers’ lives. We’ll outline some of the more interesting applications that we noticed in business, health, food, and entertainment.

AI is often used in business conferencing settings, incorporated into cameras and conferencing software. In providing different video conferencing display options like Smart Gallery, AI helps detect participants’ faces and displays them in equal proportions, facilitating an efficient, natural communication process. By ensuring that the face of each participant is visible to everyone, participants can communicate more freely and clearly.
Also, more businesses like Aira are creating AI facial recognition solutions for surveillance and workforce management systems. Placed at an entrance, the AI systems are applied in contactless access control, capable of recognizing employees, maintaining attendance records, registering visitor information, and identifying VIPs and blacklisted individuals. Some systems even include fever screening to maintain healthier work environments.

For patient-doctor communication, AI applications exist in medical cameras to improve doctor-patient communication in telehealth. As acoustics during a telemedicine session can affect the communication process and sometimes even the diagnosis, AI use in acoustics reduces unwanted noise and provides clearer audio to improve communication. These cameras have high-quality audio and high-resolution lenses for the best presentation of details, so doctors can make better clinical decisions for their patients.
Because of the pandemic, many brands like MSI have spent time and resources developing disinfection robots for indoor areas. Many machines incorporate AI for site surveys, navigation route planning, human detection, and air and surface UV sterilization. This easily keeps the indoors clean and safe from viruses and bacteria, and in the future, people could potentially apply the technology to other special sites that would require disinfections, like hospitals or laboratories.

Some brands are creating machines that sort food in the preliminary stages of food production. When raw materials such as coffee beans are obtained, they often need to undergo a selection process to eliminate beans with deficiencies like discoloration, fermentation, mold, and insect damage. Workers that do this manually would need to undergo repetitive work for long hours, which is time-consuming and mentally draining. An AI bean sorter would then organize the beans into good and defective beans automatically and accurately, eliminating the painful process of handpicking good and defective beans before roasting. This type of technology can be leveraged in other food processes in the future for factory quality control and other selection processes.
In restaurants, food ordering and preparation could be automated through AI, with companies like LaFresh creating kiosks equipped with multilanguage AI voice recognition so customers can speak to place orders. For store management, AI can calculate and forecast food usage, and in turn, reduce food waste and financial waste. AI can create and optimize complex processes in any food industry application, assisting to sift through large amounts of data efficiently and automatically.

For live performances, AI camera tracking technologies can follow specific performers to automatically stream and film performances without manual operation. These cameras can operate under different tracking modes, automatically adjusting the framing to catch the best angles of the performance.
On video platforms like YouTube, many have incorporated AI into their video screening process, helping workers to flag or remove inappropriate content. Though not perfect, it undoubtedly processes a significant amount of video content quicker than a human does, speeding up the identification of videos that do not comply with platform standards.
In gaming, generative AI can now be used to assist game developers in building NPC characters, creating convincing backstories and animation for the characters. This opens a whole new world to gamers as the games are no longer strictly limited to what the developers’ script says, allowing games to unfold with many more possibilities.
We’ve only mentioned a few uses of AI in four select areas, but in the future, there will be many more use cases in all industries, streamlining different areas of our lives. Soon, we could be using AI voice control to automate camera operations during a video conference or presentation, employing AI image analysis to support medical examinations and food processing, and utilizing AI to create videos, movies, and games. In the distant future, the applications of generative AI could be even more extensive and bring even greater convenience to our lives. With these possibilities in mind, which AI applications are you the most excited about?
Last Updated: June 20, 2024

Maggie Chu is a Brand Communication Strategist at AVer Information, working out of Taipei, Taiwan. She crafts press releases, blog posts, and other marketing materials to support AVer’s global branding efforts. She has a black dog named Niuniu, who is ironically a scaredy cat.
By Willis Leo
The image of an ICU nurse vigilantly monitoring patients has long been the cornerstone of intensive care. However, the healthcare landscape is changing rapidly, and with it, the very boundaries of where critical care is delivered.
In this article, discover how tele-ICU improves patient outcomes, expands care access, and offers work-life balance for nurses. Learn about challenges, best practices, and the technology shaping the future of intensive care.

Fundamentally, there are three main uses for Telemedicine: (1) extending coverage (e.g. Critical Access Hospitals (CAH) providing care to patients who would otherwise have limited access to specialists); (2) improving compliance (monitoring patients’ adherence to treatment plans); and (3) facilitating transfers (when specialists consult with one another on transferring a patient to another facility).
Tele-ICU nurses leverage real-time video and audio feeds from strategically placed cameras to remotely review medical records, analyze data, interpret vital signs, tackle complex patient situations with colleagues, and perform routine and unscheduled patient surveillance.
For telehealth practitioners, remote patient monitoring (RPM) offers a unique path to career development and specialization. Moreover, tele-intensive care provides greater flexibility and work-life balance than traditional settings, which appeals to nurses who want a different work dynamic. Meanwhile, offsite help can reduce stress for bedside nurses by providing additional support and expertise to ease workloads.
While tele-intensive care offers numerous benefits for an organization, it also presents unique challenges:
To address these challenges, leadership support is needed to successfully integrate the virtual and on-site teams. Drawing from case studies, some proven strategies include:
Leadership buy-in and understanding the challenges are a great start, as are technological considerations that enable tele-ICU nurses to reach their full potential.

The integration of technologies like AVer’s PTZ cameras in tele-ICU settings, as seen in a private hospital in New Taipei City, highlights the broader trend of how advanced equipment is transforming ICU nursing. PTZ cameras, like AVer’s medical-grade certified IEC 60601-1-2, offer two-way communications and minimize the need for nurses to move frequently between stations. By streamlining workflow, nurses can spend more time directly helping patients, potentially leading to lower mortality rates and shorter hospital stays thanks to timely interventions.
Beyond audio-visual advancements, other technological innovations are also making significant contributions. For instance, wearable patient monitoring devices and automated medication dispensers reduce manual tasks and minimize medication errors; smart beds gather real-time patient movement data and vital signs; and remote telemetry enables continuous cardiac monitoring. Integrating these devices with electronic health records (EHR) software is key to smoother care coordination and reducing miscommunications during shift handovers.
Collectively, these technologies not only streamline operations but also allow nurses to focus on intensive care tasks, enhancing patient outcomes through earlier intervention and more informed decision-making.
As the global focus on patient care intensifies, so does the pace of advancements in healthcare, telehealth technologies, and an emphasis on healthcare reforms. Across Europe, substantial investments in healthcare infrastructure, exemplified by initiatives like the UK’s NHS Long Term Plan, Italy’s national health system upgrade, and Germany’s Hospital Future Act (KHZG), signal a movement toward integrating advanced healthcare technologies as well as digitalization and modernization of national healthcare system. The future of tele-ICU and healthcare in general is poised to be as transformative as it is inclusive, moving us closer to a reality where quality healthcare knows no boundaries. Explore how AVer’s Connected Health Solutions offer a win-win for everyone involved and the future of the ICU.

Willis Leo is a Brand Communication Strategist at AVer Information, working out of Taipei, Taiwan. He crafts press releases, blog posts, and other marketing materials to support AVer’s global branding efforts.
By Emily Lee

With medical science and technology advancing at an increasingly rapid rate, it is more important than ever that doctors, nurses, and support staff stay up to date with continuing medical education. Continuing medical education (CME) can refer to educational activities which help to maintain and increase the knowledge, skills, and professional performance of medical health professionals. This can be in the form of formal courses, seminars, lectures, online classes, and workshops.
In this article, we examine the evolution of CME and current CME trends, investigating the shortcomings of the current methods and overcoming them by leveraging technologies such as telehealth cameras.
Over the years, CME has evolved from traditional, in-person lecture-based formats to dynamic, technology-enhanced learning experiences. Studies have shown live media to be more effective than print and multimedia formats more effective than single-media formats.
The ongoing advancement of educational research and technologies paves the way for more innovative and interactive delivery methods, including:

Despite the aforementioned advancements in CME, significant challenges in continuing medical education remain for medical professionals, highlighting the ongoing need for improvements to ensure and sustain physician competency and performance.
According to the ACCME, a professional practice gap is defined as the “difference between current health care processes or outcomes observed in practice, and those potentially achievable on the basis of current professional knowledge”.
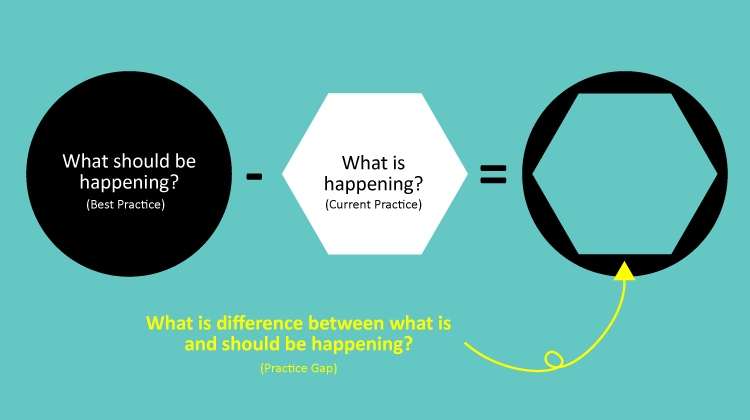
A practice gap can be categorized into one or more of the following types:
Through performing gap analyses, medical professionals can effectively understand and begin to reduce the practice gap through CME, enabling the identification of areas for improvement and ultimately the achievement of improved patient care and safety.
Aside from practice gaps, medical professionals face many barriers to accessing Continuing Medical Education (CME). A 2021 survey with US clinicians indicates that expenses and travel time are the main barriers to CME, with 68% citing costs and 57% highlighting travel time as a significant concern.
With the existing barriers, medical professionals might be restricted from accessing the educational resources they need, thereby limiting their physician competency and performance.
“We should explore options that reduce barriers of time and money, and creatively use online tools to publicize new offerings.”

To solve the issues that medical practitioners face, CME has been moving online to improve accessibility, relying heavily on commercial general-use devices such as smart glasses and video conferencing cameras to satisfy the extensive demand for recording or streaming CME content. Medical professionals found several notable disadvantages when using these devices, including unstable image quality, the need for an additional audio device, and the inability to zoom in and capture the intended view. These limitations restricted the delivery of educational content.
When the pandemic struck, telehealth cameras were suddenly thrust to the forefront of the medical industry. Having undergone significant technological upgrades, telehealth cameras are being integrated into CME, most notably its use in surgical live-streaming, marking a pivotal shift in how medical education is delivered.
Applications of telehealth cameras in CME now include:

Emily Lee is a Brand Communication Strategist at AVer Information, working out of Taipei, Taiwan. She crafts press releases, blog posts, and other marketing materials to support AVer’s global branding efforts.
Click one of our contacts below to chat on WhatsApp